Do you ever feel exhausted in the morning, no matter how many hours of sleep you put to bed each night?
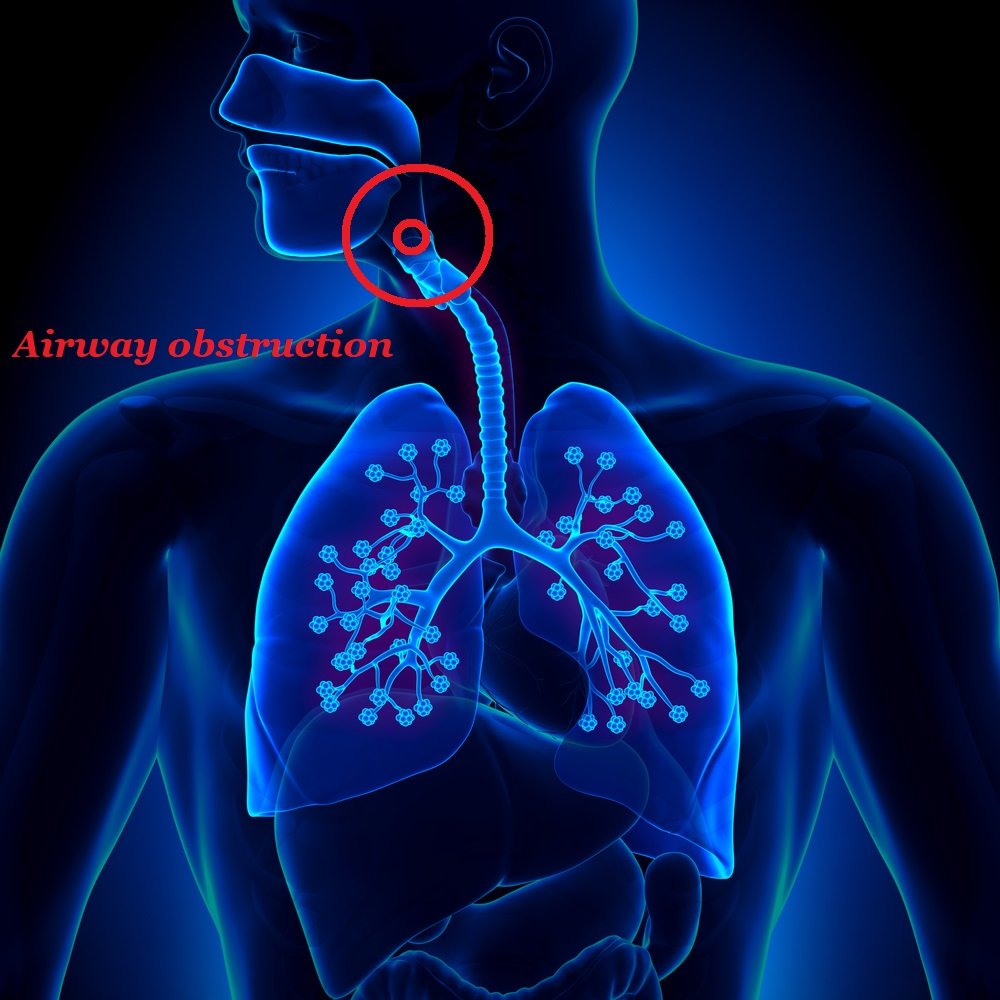
The truth is that there are about 900 million of people all over the world that feel this way. The cause: obstructive sleep apnea (OSA), a debilitating sleep disorder that continuously obstructs breathing during sleep, sometimes causing pauses of up to one minute.
What happens to you during episodes of obstructive sleep apnea is that your airways collapse and prevent breathing, starving the brain out of oxygen and involuntarily waking you up, without you even realizing what just happened.
In the morning you feel utterly exhausted, as if you haven’t slept at all; despite going early to bed and waking at 9 am.
Unfortunately, many sleep apnea sufferers have absolutely no idea that they have a serious disorder preventing them from a normal restorative sleep. They have no idea how many sleep apnea event per hour affected them either, nor they have an idea that their blood oxygen level (O2 saturation) was going up and down all night, thanks to OSA.
What can you do to see if your oxygen levels are in the healthy range?
The answer: you can monitor your blood oxygen levels with a pulse oximeter.
- Lowered oxygen saturation is anything below 96%.
- Oximeters calculate O2 saturation by measuring blood oxygen levels
- Oxygen saturation measuring analyzes the percentage of oxygenated hemoglobins within red blood cells.
The method is completely non-invasive; you simply put the pulse oximeter on your finger, and it scans your skin with red ligh. Then the device provides an instant answer as to whether your saturation is in the normal range or not.
What is hypoxemia?
During severe sleep apnea episodes, the levels can go below 79%, while moderate apneic events often lower your O2 levels below 90%, causing hypoxemia. Hypoxemia is expressed through symptoms like breathlessness and irregular breathing. If that sounds familiar, do not wait and seek help from your healthcare provider as soon as you can.
So don’t sacrifice your good night’s sleep and learn if your blood oxygen levels are in the healthy range! The solution for that is already here and it’s called pulse oximeters.
How to understand sleep apnea using pulse oximeters?
Lowered blood oxygen levels may lead to a series of health complications such as heart disease, diabetes, high blood pressure and depression to name a few.
When you are tested for sleep apnea, pulse oximetry will be used by your sleep doctor in order to learn exactly how often your breathing stops when you sleep. The oximeter will precisely show how your oxygen saturation and heart rate is affected by apneic events by directing a wavelength of light to your finger.
The changes are carefully recorded and analysed by your sleep doctor in the morning, when they examine the results and determine whether you have OSA and its severity.
In short, if you experience frequent drops in blood oxygenation, then it is very probable than you suffer from obstructive or central sleep apnea.
Blood oxygen levels: what is safe and what is not?
If your oxygen saturation falls under 92%, it may signify that a breathing problem is causing the drop. This could mean that you have obstructive sleep apnea or another disorder like asthma or COPD.
The most important factor in deciding whether these drops are really problematic or somehow normal, is understanding their continuity; that is how long are these oxygen drop events that you are experiencing every night. They can be short ones (considered normal) or prolonged ones, with serious complications for your health.
If you decide not to schedule an appointment with a sleep specialist and undergo this kind of screening at their lab, you can definitely use a pulse oximeter and self-monitor your sleep at the comfort of your home.
Pulse oximeters: affordability vs. reliability
Fortunately, pulse oximeters are very affordable and reliable when it comes to monitoring your O2 levels. They can help you understand that there is an underlying cause for these drops and, and that sleep apnea is the possible culprit for these. Or you can decide to take matter in your own hands and seek professional help.
Continuous positive airway pressure therapy is the golden standard in treating sleep apnea, but before you even start with it, you need to take the first step towards understanding what’s happening to your body and how exactly it affects your daily life.
Pulse ox utilization: pre-nighttime diagnosis, after initial diagnosis and during ongoing treatment
Pulse oxs find direct utilization in diagnosing sleep-disordered breathing in OSA, becoming an essential tool in both clinical and home sleep diagnosis. This is particularly effective in monitoring sleep apnea before nighttime blood oxygen desaturation, during initial diagnosis and ongoing treatment. Out of any other blood O2 monitoring methods, pulse ox devices have become the gold standard when it comes to obtaining a sustainable degree of accuracy across the large majority of patients suffering from apnea. With the latest advance in pulse ox technology that accuracy rate has jumped significantly.
Pulse oximetry is the most essential blood oxygen monitoring method during CPAP therapy; and it can help in setting up the best air pressure level and flow for the particular need. However, oximetry is not enough to diagnose OSA just by monitoring O2 levels. In this sense, although essential in the diagnosis, pulse ox devices come as auxiliary monitoring method requiring corroboration with other standard data-acquisition techniques in OSA screening. Furthermore, O2 measurement of this kind may give false negatives or positives, which is why it needs to be paired with other diagnostic techniques. The accuracy of pulse oximeter units is also subject to other underlying health conditions (diabetes) or bad habits such (smoking).
In the US the requirement for qualifying with sleep apnea is a registered drop of 4% in blood oxygen levels, although even a smaller percentage of 2% may indicate a serious clinical condition that requires immediate attention. Immediate CPAP therapy is not required, but further testing needs to be done in order to identify the problem and if indeed is OSA-related or not.


